
在2016年中原心脏病学大会中,Ihor Gussak教授带来了题为“Drugs in Acutely Decompensated Heart Failure: Lesions to Learn ”的精彩报告

DISCLAIMER
声明
The opinions expressed in this presentation do not
necessarily represent the views of:
◆Rutgers University or
◆Office of the Journal of Electrocardiology
这里表达的观点不代表以下单位的观点:
美国罗格斯大学或心电生理杂志
Introduction 引言
Quotes from Dr. Eugene Braunwald (2013)*引用Eugene Braunwald博士2013年研究
◆Despite major improvements in the treatment of virtually all cardiac disorders, heart failure (HF) is an exception, in that its prevalence is rising, and only small prolongations in survival are occurring
尽管所有的心血管病的治疗都在提高,但是心衰是一个例外,也就是说它的发病率在增长,目前仅有小部分人的生存得到延长。
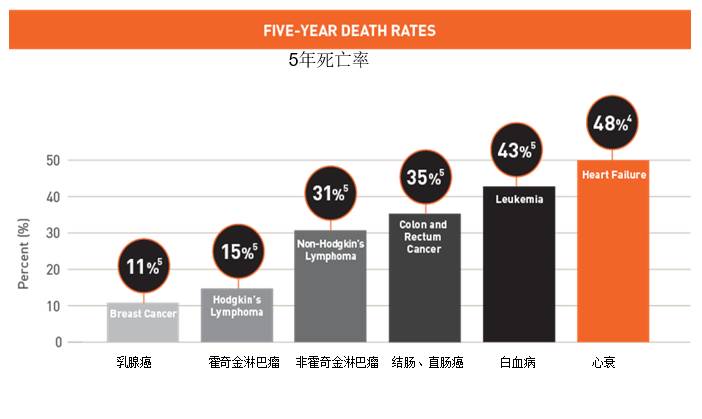
◆5-year mortality is still ~ 50%, worse than that of many cancers
5年生存率比某些癌症更糟糕,仍旧低于50%。
◆> 50% of the total cost of HF in the U.S. is due to ADHF hospitalization, while only ~10% of the total cost of HF in U.S. is due to pharmacological treatment
在美国,大于50%的心衰费用是用在急性失代偿性心衰的住院治疗,然而只有10%的心衰费用是用在药物治疗上。
◆None of the existing treatments has ever been shown to be both safe and efficacious by modern standards (e.g. randomized controlled trials)
按现在标准没有任何现有的治疗是被证明安全的、有效的(如随机对照试验)
◆Over the last decades, attempts to develop new therapies for acute HF or ADHF have largely failed
在过去的几十年里,尝试发展急性失代偿性心力衰竭或急性心衰新的治疗,基本都上失败了
[1][2]
Open Questions / Dilemmas问题/困境
1.Why mortality in ADHF is so high and almost the same over decades, while mortality from ACS (AMI) is reduced by 75%?
为什么急性失代偿性心衰的死亡率数十年一直这么高,然而急性心梗的死亡率减少了75%
2. What was not done right and what can be done differently in the future?
什么地方做的不对,将来我们能做些什么不同的吗?
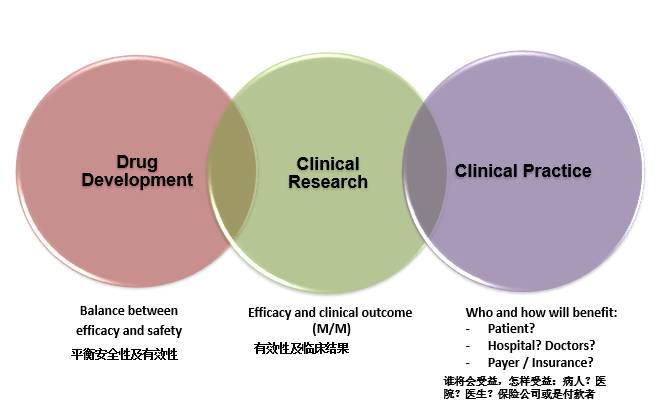
The aim of this presentation is to review the challenges in development and implementation of the drug therapies for ADHF in:
本课的目的是回顾急性失代偿性心衰的药物治疗在以下方面的挑战
◆clinical practice, 临床实践
◆drug development, 药物发展
◆clinical research临床研究
Clinical Practice vs Clinical Research vs Drug Development
临床实践 VS临床研究VS药物发展
Heart Failure: Syndrome vs Disease
心衰:症状VS疾病
◆Both CHF and AHF are complex clinical syndromes (not diseases) of 慢性心衰和急性心都是一个复杂的临床症状
—Multiple etiologies, co-morbidities, triggering and participating factors
多病因,副发症,诱发和参与因素
—Various structural, functional, and biologic alterations
结构,功能和器质性改变
—Pathophysiology, treatment, and prognosis
病理生理、治疗和预后
defined as (chronic or acute) impaired ability of the heart to maintain an adequate circulation of oxygenated blood and nutrients to the peripheral tissues to meet their metabolic demands due to deterioration of:
心衰的定义是:急性/慢性原因所致心脏不能将氧合血液和营养运输至外周组织来满足外周组织代谢需要,原因包括:
—Contractility function of the heart (systolic dysfunction) and/or 收缩功能
—Cardiac elasticity and relaxation (diastolic dysfunction) or舒张功能
—Both两者都有
◆Most common causes: 共同原因
—CAD with or without MI冠心病 有或无心梗
—Primary cardiomyopathies (dilated or hypertrophied)原发心肌病(扩张性或是肥厚性)
—Secondary cardiomyopathies (toxic, post-infectious, end-stage pressure overload)继发心肌病(中毒,感染,晚期压力负荷过重)
◆Common mechanism - progressive structural damage of the heart associated with:常见机制——与心脏结构损害相关:
—Replacement of the functionally active myocardial tissue by fibrotic tissue and功能活跃的心肌被纤维组织替换
—Hypertrophy of remaining myocytes (myocardial remodeling)肥厚的心肌(心肌重塑)
IG: HF is a “certain uncertainty”
ADHF vs AHF: Clinical Spectrum急性失代偿性心衰VS急性心衰:临床表现
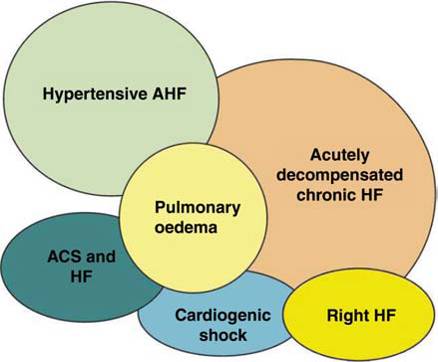
“Common Pathway” for ADHF
急性失代偿性心衰共同通路
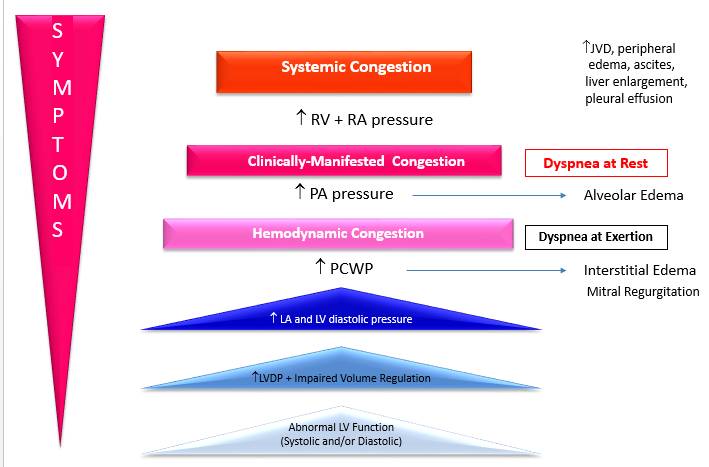
◆The hallmark of ADHF is acutely decompensated CV (HD) congestion
急性失代偿性心衰的特点是急性失代偿性肺静脉淤血(体循环淤血)
◆HD congestion (symptoms and signs of increase filling pressure and volume) are commonly due to体循环淤血共同由于(增加的充盈压和血容量的症状和体征)
—Increase volume (body weight, pedal edema, ascites, pleural and/or pericardial effusions)增加容量(体重,脚肿,腹水,胸腔/心包积液)
—Redistribution of volume (LV HF)血容量重新分配(射血分数保留心衰)
—Both (bilateral HF)两者都有
◆The major factors underlying pathophysiology of ADHF include:
急性失代偿性心衰根本病理生理机制关键因素包括:
—Impaired cardiac pump function (systolic failure) and/or abnormal loading/filling conditions (diastolic failure) that are associated with:
和心脏泵血功能受损(收缩功能衰竭)和/或超负荷/充盈受损(舒张功能障碍)相关
—Neurohormonal and circulatory abnormalities, including sodium and fluid retention by kidney, resulting in development of shortness of breath (dyspnea) and fatigue upon exertion and/or at rest
神经体液异常包括肾脏的水钠潴留,导致在静息/活动时呼吸困难。
◆Treatment of symptoms of congestion is not a cure of underlying disease
治疗充血症状不代表治愈原发病
[3]
Epidemiology of HF and ADHF 心衰和急性失代偿性心衰的流行病学特征
HF: Epidemiology心衰:流行病学
◆More than 23 million people with HF worldwide:
世界上超过2.3亿人有心衰
—6 million - in USA, 10 million – in Europe, and 1 million – in Japan
—Prevalence - 0.5-2% of the population, - 0.9% - in China
—The lifetime risk is 1 in 5 for both males and females
◆670,000 individuals are diagnosed with HF for the first time each year in USA
在美国,每年有670000个体诊断为心衰
◆Incidence ~ 1% after age 65 and continues to rise with:
—Aging of the baby boomer generation
—Increased prevalence of risk factors for HF
—Improved survival rate after MI
◆ADHF is the most common cause for hospitalization in 65y+ patients
急性失代偿性心衰是65岁以上病人住院最常见的原因
◆More than 1 million hospitalizations annually in USA
—Median duration of hospitalization - 6 days, 11.3 days – in China, and 28 days - in Japan
—Subsequent 6 months of re-hospitalization rate - 50%
HF: Epidemiology (2)
◆5-year survival rates in HF population is 50%
心衰5年生存率是50%
—Despite well-established yet limited clinical benefits of ACEI, ARB, and BB
尽管目前有临床受益有限的ACEI、ARB和β受体阻滞剂
—1 in 5 newly diagnosed patients with CHF dying within 1 year 有五分之一的新确诊的慢性心衰病人在一年内死亡
◆2-year mortality rate in end-stage HF is 70-80%
终末期心衰的2年死亡率是70-80%
—Affects over 60,000 people in USA each year在美国每年影响超过6万人
—Treatment options are limited:有限的治疗选择
<3,000 heart transplants per year
Implantable Left Ventricle Assist Devices (LVADs) are not for long-term support
◆Low medication compliance 药物依从性低
◆Direct and indirect cost in USA only: >$30 billion per year (2005)
在美国,仅仅是直接和间接花费每年大于300亿美金(2005)
Current Standard of Care 目前的治疗标准
HF: Classifications心衰:分类
◆NYHA (functional class: I, II, III, IV)纽约心脏病学分级(I、II、III、IV功能分级)
—This score documents severity of symptoms
—Can be used to assess response to treatment
—Is not very reproducible and doesn't reliably predict the walking distance or exercise tolerance
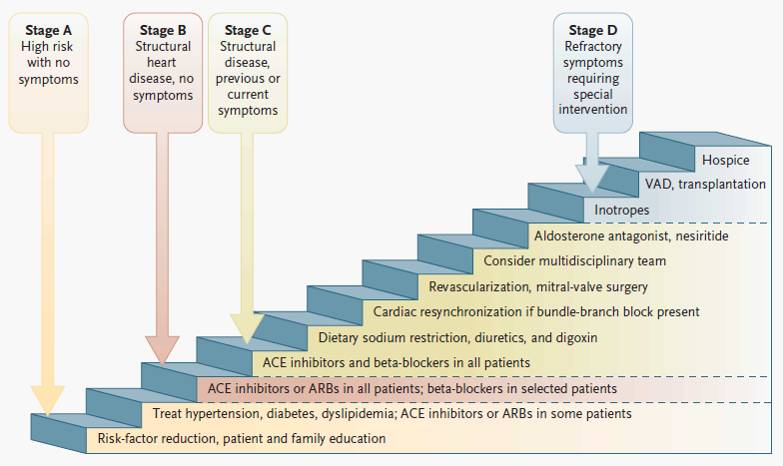
◆ACC/AHA (progression stage: A, B, C, D)
美国心脏病学会/美国心脏病协会(进展分期)
—Stage A does not have a corresponding NYHA class
—Stage B would correspond to NYHA Class I
—Stage C corresponds to NYHA Class II and III
—Stage D overlaps with NYHA Class IV
◆High and Low output 高低输出量
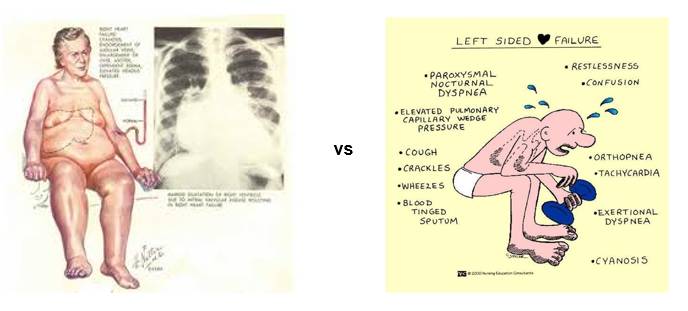
◆Left-sided vs Right-sided vs Total (bilateral) 左心衰VS右心衰VS全心衰
◆Systolic vs Diastolic 收缩功能VS舒张功能
◆Post-MI vs CHF 陈旧性心梗VS慢性心衰
◆ADHF vs AHF急性失代偿性心衰VS急性心衰
◆Intracellular or Interstitial细胞内或细胞间
HF Stages and Treatment Strategy心衰的分期和治疗策略
[4]
Standard of Care in CHF and ADHF慢性心衰和急性失代偿性心力衰竭治疗标准
Treatment of CHF (at home)
—ACE inhibitors and/or ARBs
—β-blockers
—Aldosterone antagonists
—Diuretics
—Optional (add-on treatments):
●Digitalis
●BiDil
院外慢性心衰的治疗:
1、ACEI或ARB
2、β受体阻滞剂
3、醛固酮受拮抗剂
4、利尿剂
5、选择(附加治疗)
洋地黄
肼苯哒嗪75mg+消心痛40mg
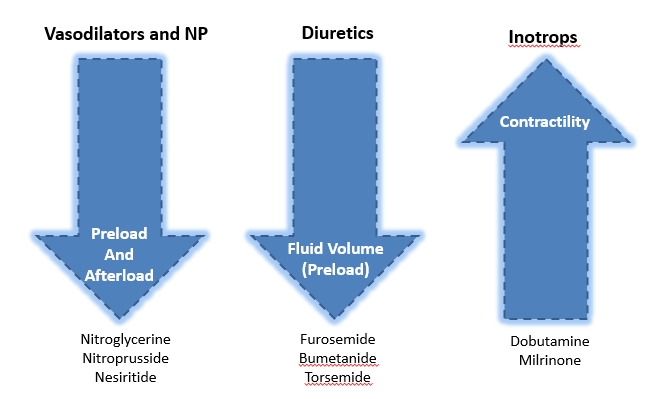
院外急性失代偿性心衰治疗:
1、血管扩张剂(硝酸甘油或奈西利肽)
2、袢利尿剂(呋塞米或布美他尼)
3、强心剂(多巴酚丁胺,米力农)
4、氧气
5、吗啡
6、机械通气
Treatment of ADHF (at hospital)
—Vasodilators (nitroglycerin or nesiritide)
—Loop diuretics (furosemide, bumetanide)
—Positive inotropis (dobutamine, milrinone)
—Oxygen
—Morphine
—Mechanical ventilation
Therapeutic Strategy in ADHF急性失代偿性心力衰竭治疗策略
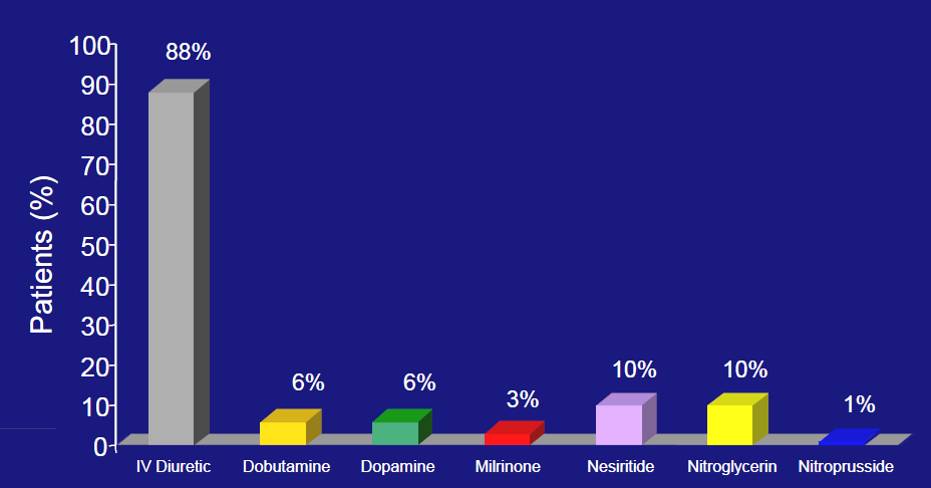
Most Common I/V Drugs in ADHF(based on 2004 ADHERE registry)
Adverse Effects of Diuretics 利尿剂的不良反应
◆High-dose diuretic therapy is a marker for increased mortality during hospitalization for ADHF, similarly to its use for CHF:同慢性心衰一样,急性失代偿性心衰住院期间用大剂量的利尿剂是增加死亡率的标志
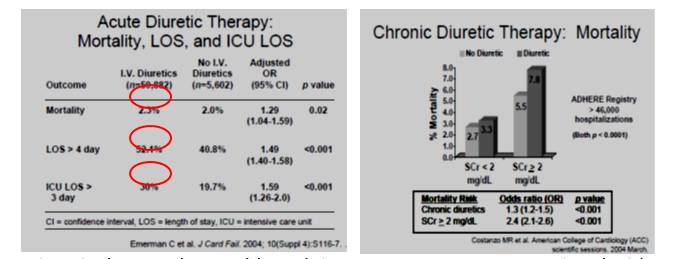
◆Diuretic therapy that could result in poor outcomes are associated with:
利尿剂引起的不良后果于以下因素相关
Electrolyte disturbance, hypotension, volume depletion, and worsening renal function
◆Mechanism is unclear: 机制尚不明确
Whether this is a direct adverse effect of diuretics or a reflection of the severity of the HF
Diuretics for Both?
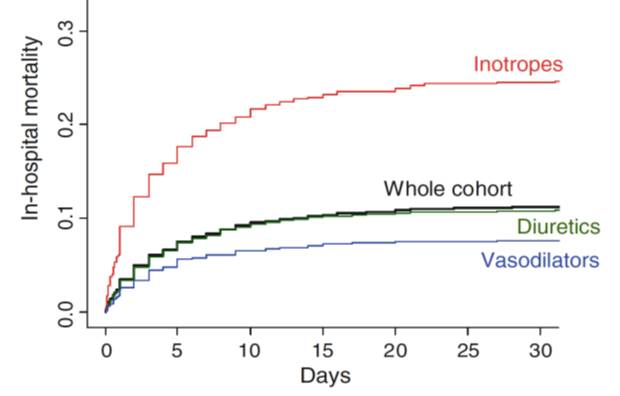
Current Drug Therapies and In-hospital Mortality目前的药物治疗和住院死亡率
Existing Drug Therapies in ADHFADHF目前药物治疗 (Summary)
Current treatments that effectively relieve symptoms in ADHF (diuretics, vasodilators, inotropes, morphine) are associated with significant short-term and even long-term adverse effects on renal and CV functions:
目前能有效缓解ADHF症状的治疗(利尿剂、血管舒张、吗啡),与长期或是短期肾功能或是心血管功能的不良反应有关
↑ SCr 肌酐
↑ Hypotension, tachycardia 低血压、心动过速
↑ Electrical instability 心电不稳定
↓Mortality / Morbidity死亡率/发病率
Unmet Medical Needs For New Drug Therapies未满足的医疗需要新的药物疗法
[5]
◆High (and virtually unchanged over decades) mortality and re-admission rate
高死亡率(几十年几乎不变)和再入院率
◆Unsatisfied efficacy of existing drugs:
目前药物效果不满意
—60% ADHF patients discharged home with dyspnea or fatigue
—45% ADHF had worsening HF within 60-days post-discharge and 25% ADHF had to be re-admitted within 60-days post-discharge*
◆Unsatisfied safety of existing drugs
目前药物安全性令人不满意
◆High cost:
花费高
—More that 50% of the total cost of HF in the U.S. is due to hospitalization, while nearly 10% of the total cost of HF in U.S. is due to pharmacological treatment
—Hospitalization is expensive, accounting for approximately 80% of the estimated $24.7 B in direct costs for HF care in the U.S. only, and global economic burden for HF exceeds $45 B USD (or 2% of global healthcare expenditure)
—Interest in re-admission to the hospital due to ADHF has skyrocketed in the U.S. since the Patient Protection and Affordable Care Act (PPACA, 2010) called for institution of hospital payment penalties by the Centers for Medicare and Medicaid Services (CMS) for excessive 30-day all-cause re-admission rates following index hospitalization for HF, acute MI, or pneumonia**
Clinical Research and Drug Development in ADHF 急性失代偿性心衰的临床研究及药物发展
Clinical Research and Drug Development: Structure and Challenges临床研究和药物发展:结构和挑战

Clinical R&D临床研究
◆Phase I: safety, tolerability, PK and PD in HV
1期:安全性,耐受性,
—Pharmacology/Pharmacokinetic studies (DMPK, Bioavailability)
—Maximum tolerated dose study
◆Phase II: dose-ranging, dose-finding studies
2期:药物剂量范围,剂量探索研究
—Safety, tolerability, PK and PD in patients
—MoA, Proof of Principle, Proof of Concept
◆Phase III (“shift” from safety to efficacy):
3期有效性与安全性的转换
—Non-inferiority (registration) studies over placebo when added to current approved therapy in target population
◆Phase IV: post-marketing
4期上市后
—Superiority studies over placebo, existing therapies and competitors, extension of indications
Profile of “Ideal” Drug for ADHF
◆Substantial (a) improvements/alleviation of ADHF signs and symptoms (e.g. dyspnea) at rest, with minimal activity, or at exertion and (b) to reduce all cause in-hospital mortality
显著改善/减轻ADHF静息时的呼吸困难时的症状和体征,或者减少活动,减少住院时全因死亡率。
◆Acceptable safety and efficacy irrespective of: 可接受的安全性和有效性不考虑:
—Pathogenesis of HF
—LVEF
—Arterial BP
—Renal and/or hepatic impairments
◆Rapid onset and durable effectiveness and no rebound effects
快速起效、长效、不反弹效果
—No worsening of ADHF symptoms and signs
—No cardiac or renal damages or deteriorated functions
—No pro-arrhythmia and/or ischemia
—Improve the neurohumoral profile, diastolic and systolic dysfunction, systemic vascular resistance, cardiac output without adverse effect on the HR and arterial BP
◆Reduce diuretic and/or inotropes doses or remove the need for this therapy
Reduction in LoS and post-discharge morbidity and mortality
减少出院后发病率和死亡率
◆Complementary and not contraindicative to drugs used to treat CHF:慢性心衰药物治疗的互补作用而不是禁忌
—No DDI and/or DFI
—No interactions with OTC medications
Challenges and Dilemmas in Clinical R&D R&D临床研究的挑战和困难
◆Disconnects (Gaps) Between:差距
—Positive Phase II does not necessary “translate” into successful Phase III
—HD studies and exercise studies (Phase II) are helpful in assessing the MoA and/or dose selection yet not predictive of success in Phase III (except HR and LV volumes)
◆Individual (safety and efficacy) responses vary significantly and depend on:
个人(安全性和有效性)反应显著不同,取决于:
—Stage of HF
—Underlying mechanism of HF
—Concomitant medications and accompanying diseases (cardiac, renal, and liver failures) that also significantly impact the sample size of clinical trials
◆Large, long, and costly outcome studies
大量、长期、珍贵的研究结果
—“Soft” and “intermediate” surrogate markers (e.g. alleviation of symptoms, reduction in PCWP) are not sufficient enough to register the product
—Lack of biomarkers that have been validated as surrogates for mortality and morbidity
—“End-point driven” trials generally require a long follow and large number of patients
Summary, Conclusions, and Future Trends in ADHF 急性失代偿性心衰的总结、结论及未来发展趋势
Drug Therapies in ADHF(Summary) ADHF药物治疗总结
[6]
◆Current (existing) treatments are neither safe, or effective, or both
◆Investigational drugs: no much of progress in the last 2 decades
—~ 10 agents tested in large outcome-focused, randomized trials*
—> 20 trials have been conducted in ADHF, but only one (serelaxin in Pre-RELAX-AHF and RELAX-AHF) was a disputably successful in reducing mortality (not morbidity)
—Despite promise, these studies failed to improve phase 3 outcomes**
1、目前治疗策略或者不安全或者没有效或者既不安全又没有效
2、试验药物:在过去二十年没有太多进展
Drug Therapies in ADHF (2)(Challenges in Medical / Clinical)
◆1.ADHF is not well defined
ADHF定义不明确
◆2.“Highly” heterogeneous and older target population with many
高异质性和老年目标人群有以下特征:
Significant co-morbidities
Multiple concomitant therapies, including OTC medications
Various participating and triggering factors
Low compliance with drugs and diet
◆3.Multifactorial Etiology and Pathophysiology 多因素的 病理生理学机制
—Contractility vs relaxation vs both failures
—LV vs RV vs total
—Valvular vs Congestive vs Congenital
—Interstitial fibrosis vs Loss of myocytes vs Reduced contractility function of myocytes
Drug Therapies in ADHF (3)(Challenges in Drug Development)
◆Insufficient knowledge of the MoA of the new agents
新代理人对MoA知识欠缺
◆Limited understanding of pre-clinical and clinical pathophysiology
对临床前期及临床病理生理机制缺乏理解
—Its compensatory mechanisms and
—Progression of underlying and concomitant diseases
◆Drugs interactions due to polypharmacy多种药物的相互作用
Drug Therapies in ADHF (4)(Challenges in Clinical Research)
◆1.“Gap” between pre-clinical and clinical R&D
临床前期和临床试验的差距
—Lack of valid biomarkers
◆2.“Gap” between Phase II and III
2期试验和3期试验的差距
—Lack of reliable surrogate markers
◆3.“Highly” heterogeneous population with many:
高异质群体有以下特征
—Co-morbidities
—Participating and triggering factors
—Patients/sites/countries selection for various stages of DD
—Study designs, objectives, statistical power, and execution
—High cost and length of development
Clinical R&D in ADHF: Lessons LearnedADHF临床试验的经验教训
◆Do not ↑:
—Inotropy (is not safe)
—Oxygen and metabolic needs
—Heart rate
—Electrical instability
—Aldestorone
◆Do not ↓:
—Systolic BP (avoid under-perfusion of kidney, even briefly)
—LV relaxation
◆Do not rely on symptomatic relief only
◆Consider:
—Principle: “Live longer and feel better”
—3 parties must be happy:
Patients
Doctors/hospitals
Payers (Insurance)
◆Re-admission and LoS are hottest topics at present
Instead of Conclusions 反面结论 "In theory, theory and practice are the same.
In practice, they are not“ (Albert Einstein)
理论上,理论和实践是一样的。在实践中,它们不是。
参考文献:
★ 1]Roger VL. JAMA. 2004;292(3):344-350
[2]National Cancer Institute. http://seer.cancer.gov/statfacts
[3]RV: right ventricular; RA: right atrial; PA: pulmonary artery; LA: left atrial; LVDP: LV diastolic pressure; JVD: jugular vein distension
[4]From: Jessup M. NEJM, 2003; 348: 2007
[5]Gattis, JACC 2004
** - Stone, 2010
[6] Vaduganathan. Nature Review Cardiovascular, 2013
** - Butler. JAMA, 2013
★
MD, PhD, FACC Cardiovascular ConsultantClinical Professor of Medicine, Rutgers RWJ Medical SchoolExecutive Editor, Journal of Electrocardiology