
肥胖与代谢综合征
IDF的MS标准(2005/2009+AHA)
[1]
◆中心性肥胖(必要条件)
腰围*: 华人男性≥90cm,女性≥80cm
中国人:男性≥ 85cm(2尺55),女性≥80cm(2尺4)(2009)
欧洲裔人 M ≥94cm,F ≥ 80cm(美国人仍ATPIII标准)
南亚人 M ≥90cm,F ≥ 80cm……
测量方式:肋弓下缘和髂嵴上缘的中间平面
◆合并下列4项指标中任两项
TG升高:
≥150mg/dl(1.7mmol/l),或接受针对性治疗
HDL-C降低:
男<40mg/dl(1.04mmol/l),
女<50mg/dl(1.3mmol/l)或接受针对性治疗
血压升高:
≥130/85mmHg,或诊断高血压并接受相应治疗
FBG升高:
≥100mg/dl(5.6mmol/l),或2型DM,建议对FBG≥100 mg/dl者应行OGTT
特点:肥胖中心论,人种特异
MS定义的核心组分
1.肥胖
2.胰岛素抵抗
3.高血压
4.高血糖
5.血脂紊乱(2项)
MS的病因认识:
IR/血糖中心 肥胖脂肪代谢紊乱中心论
肥胖是IR/MS的始动因素
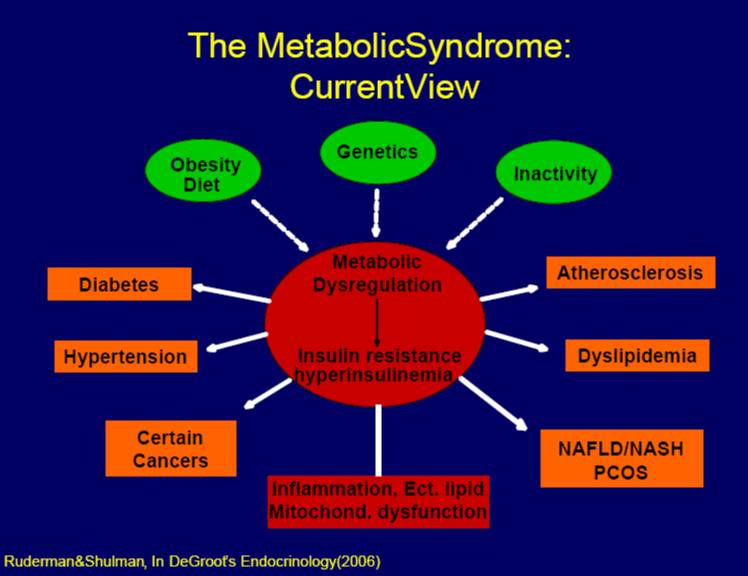
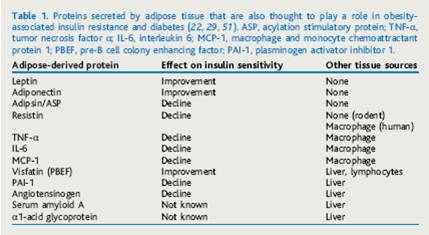
脂肪组织是炎症因子的重要来源
MS的防治
◆综合干预为主要防治手段。一级预防:生活方式干预包括减重、增加体力活动和改善不良膳食和行为习惯、戒烟
◆目前对MS的各成分的处理主要借用单一疾病的治疗模式,如何在降压、调脂、降糖、减肥和抗炎等方案组合以达到最大的效价比,值得探索
◆应该从儿童开始:结合生物标志物(脂肪因子谱)及早识别高危儿童
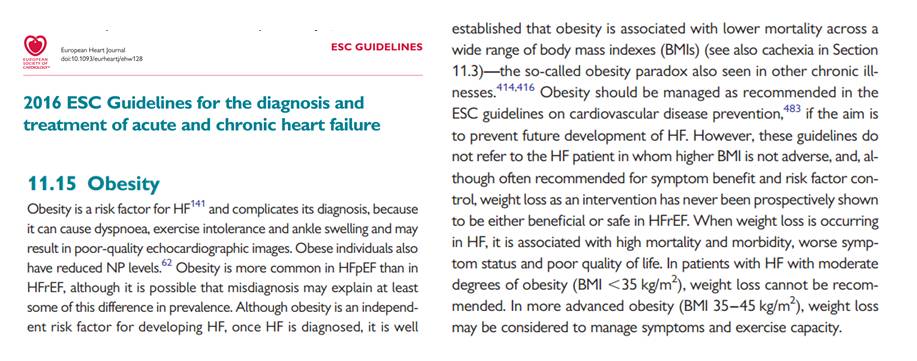
肥胖与心力衰竭
CHART研究-BMI与心衰预后呈U型曲线
[2]
这是一个多中心前瞻队列研究(2000.2-2005.12)
◆BACKGROUND:
Prognostic impact of body mass index (BMI) in Japanese patients with chronic heart failure (HF) remains unclear.
◆METHODS AND RESULTS:
We examined the relationship between BMI and the prognosis of Japanese HF patients in the Chronic Heart Failure Analysis and Registry in the Tohoku District (CHART) study. The study sample was 972 Japanese chronic HF patients (mean age, 68.2 ± 13.5; male 65.2%). We categorized them into 5 groups; BMI <18.5, 18.5 to 22.9, 23.0 to 24.9 (reference), 25.0 to 29.9, and ≥ 30.0. Using a Cox hazards model, the relationships between BMI and deaths or admission for worsening HF were studied in detail. Mean follow-up period was 3.4 ± 1.7 years. Multivariate analysis showed that, as compared with reference group (BMI 23.0 to 24.9), hazard ratios (HR) for all-cause death showed a U-shaped association with 1.70 (95% confidence interval; 1.04-2.76), 1.23 (0.85-1.78), 1.26 (0.84-1.90), and 2.75 (1.51-5.00) among those with BMI<18.5, 18.5 to 22.9, 25.0 to 29.9, and ≥ 30.0, respectively. There were significant and suggestive U-shaped associations between BMI and cardiac-cause death or admission for worsening HF.
全因死亡
1.70 (1.04-2.76), BMI<18.5
1.23 (0.85-1.78), 18.5 to 22.9,
1.26 (0.84-1.90), 25.0 to 29.9
2.75 (1.51-5.00),and ≥ 30.0。
◆CONCLUSIONS:
Both high and low BMIs were associated with increased outcomes, suggesting that extreme obesity is not beneficial in improving the prognosis of Japanese chronic HF patients.
腹围和BMI对预后的影响:肥胖悖论
[3]
◆BACKGROUND:
Higher body mass index (BMI) is associated with improved heart failure (HF) survival, but the role of waist circumference (WC) in HF outcomes has not been studied.
◆METHODS AND RESULTS:
A total of 344 patients with advanced systolic HF had WC and BMI measured at presentation. High WC was defined as ≥88 cm in women and ≥102 cm in men, and high BMI as ≥25 kg/m(2). Two-year urgent heart transplant (UT)-free survival in high vs normal WC groups was 77.9% vs 64.3% (P = .025) and in high vs normal BMI was 89.8% vs 58.2% (P < .001). After multivariable adjustment, normal WC compared with high WC was associated with higher all-cause mortality (risk ratio [RR] 2.76, 95% confidence interval [CI] 1.34-5.71) and higher risk of death/UT (RR 2.14, 95% CI 1.25-3.68). The best outcomes were seen in those with both high WC and high BMI.
◆CONCLUSIONS:
High WC, an alternative anthropometric index of obesity more specific to abdominal adiposity, high BMI, and the combination of high WC/high BMI were each associated with improved outcomes in this advanced HF cohort, lending further support for an obesity paradox in HF. The role of body composition in HF survival should be a focus of future investigation.
肥胖对于心衰的结果:男女有别
[4]
◆OBJECTIVES:
This study sought to determine whether body mass index (BMI) has a differential impact on survival for females versus males with advanced systolic heart failure (HF).
◆BACKGROUND:
Females have a survival advantage in HF, the mechanisms of which are unclear. There is also a proposed "obesity survival paradox" in which excess adiposity promotes HF survival.
◆METHODS:
We reviewed 3,811 patients with left ventricular ejection fraction ≤40% who had undergone cardiopulmonary exercise testing between 1995 and 2011. The endpoint was all-cause mortality. Multivariable analysis was performed using a Cox proportional hazards model. Because of the nonlinearity of BMI, a restricted cubic spline was used. An interaction term was added to investigate the impact of BMI on mortality by sex
肥胖对于心衰的结果:男性越胖死亡率高
◆RESULTS:
The unadjusted data demonstrated an overall obesity survival paradox in HF. This survival paradox disappeared for males after adjustment for potential confounders, with overweight and obese males showing higher adjusted mortality hazard ratios compared with normal weight males. Conversely, females in the overweight BMI range (25.0 to 29.9 kg/m(2)) had the lowest adjusted mortality (hazard ratio: 0.84; 95% confidence interval: 0.77 to 0.93; p = 0.0005 compared with normal weight females) with a nadir in mortality hazard just below BMI 30 kg/m(2). The multivariable model supported a differential impact of BMI on mortality in males versus females (p for interaction <0.0001).
◆CONCLUSIONS:
In this advanced HF cohort, an unadjusted obesity survival paradox disappeared after adjustment for confounders. Overweight and obese males had higher adjusted mortality than normal weight males, whereas a BMI in the overweight range was associated with a significant survival benefit in females.
[5]

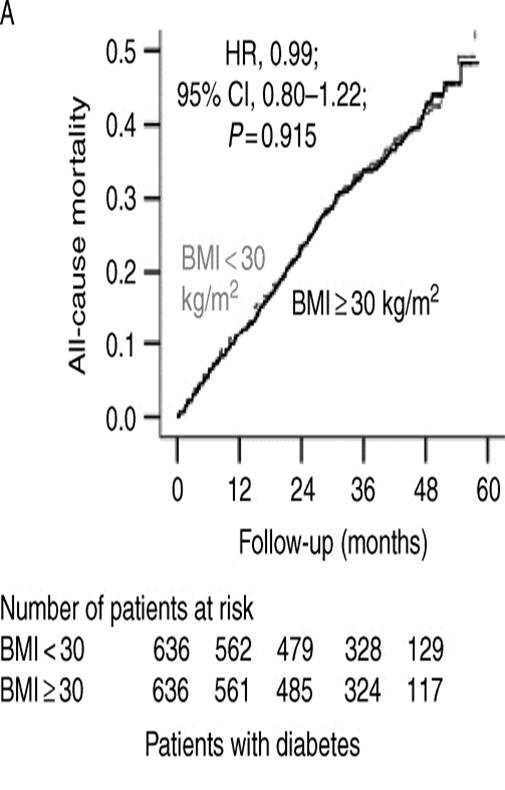
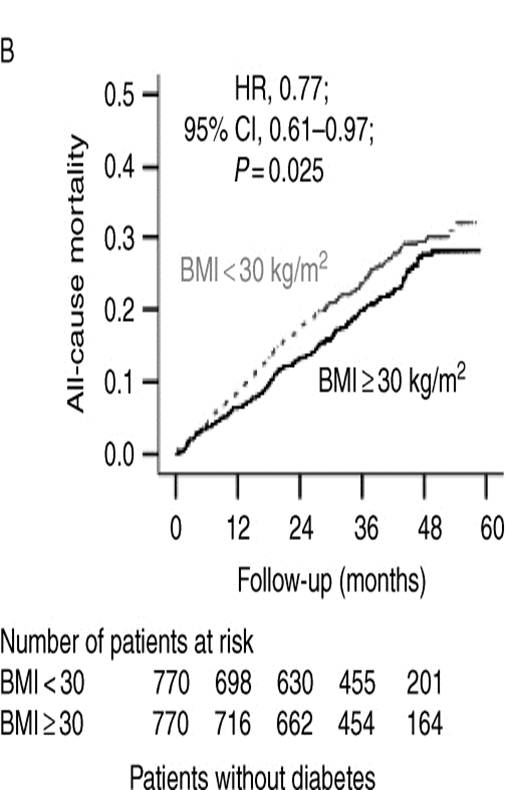
BMI与心衰预后:糖尿病打破肥胖悖论
[6]
◆Aims
Obesity is paradoxically associated with survival benefit in patients with chronic heart failure (HF). However, obesity complicates the management of diabetes mellitus (DM), which is common in HF. Yet, little is known about the impact of obesity in HF patients with DM. Therefore, we examined the association between obesity and outcomes in propensity-matched cohorts of HF patient with and without DM.
◆Methods and results
Of the 7788 participants with chronic mild to moderate HF in the Digitalis Investigation Group trial, 7379 were noncachectic [body mass index (BMI) ≥20 kg/m2] at baseline. Of these, 2153 (29%) had DM, of whom 798 (37%) were obese (BMI ≥30 kg/m2). Of the 5226 patients without DM, 1162 (22%) were obese. Propensity scores for obesity were used to separately assemble 636 pairs of obese and non-obese patients with DM and 770 pairs of obese and non-obese patients without DM, who were balanced on 32 baseline characteristics. Among matched patients with DM, all-cause mortality occurred in 38 and 39% of obese and non-obese patients, respectively [hazard ratio (HR) when obesity was compared with no obesity 0.99; 95% confidence interval (CI) 0.80–1.22; P ¼ 0.915]. Among matched patients without DM, all-cause mortality occurred in 23 and 27% obese and non-obese patients, respectively (HR associated with obesity 0.77; 95% CI 0.61–0.97; P ¼ 0.025).
◆Conclusion
In patients with chronic mild to moderate HF and DM, obesity confers no paradoxical survival benefit. Whether intentional weight loss may improve outcomes in these patients needs to be investigated in future prospective studies.
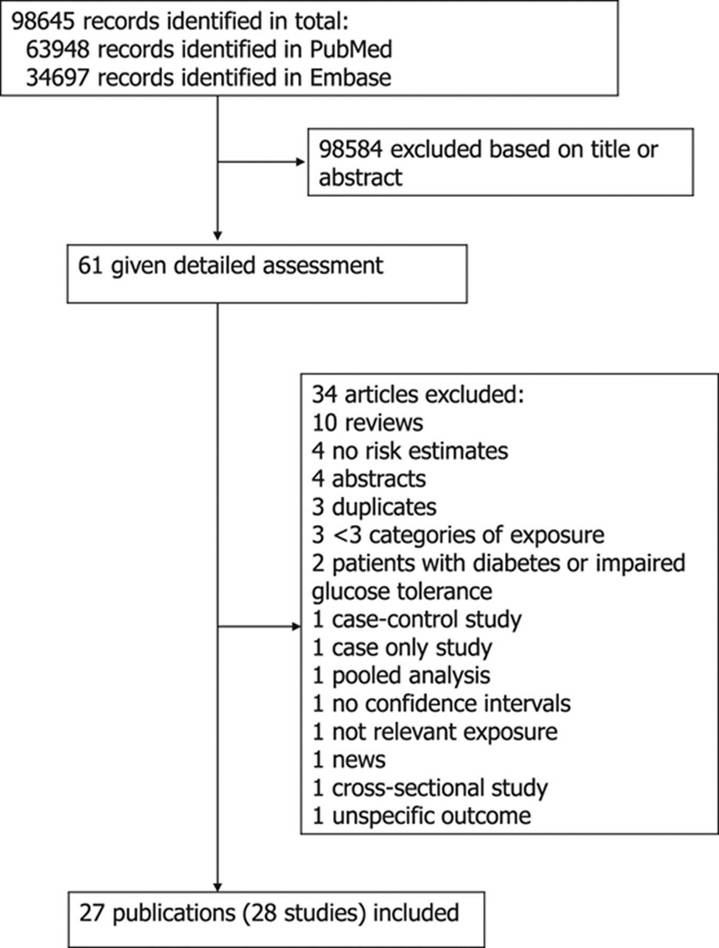
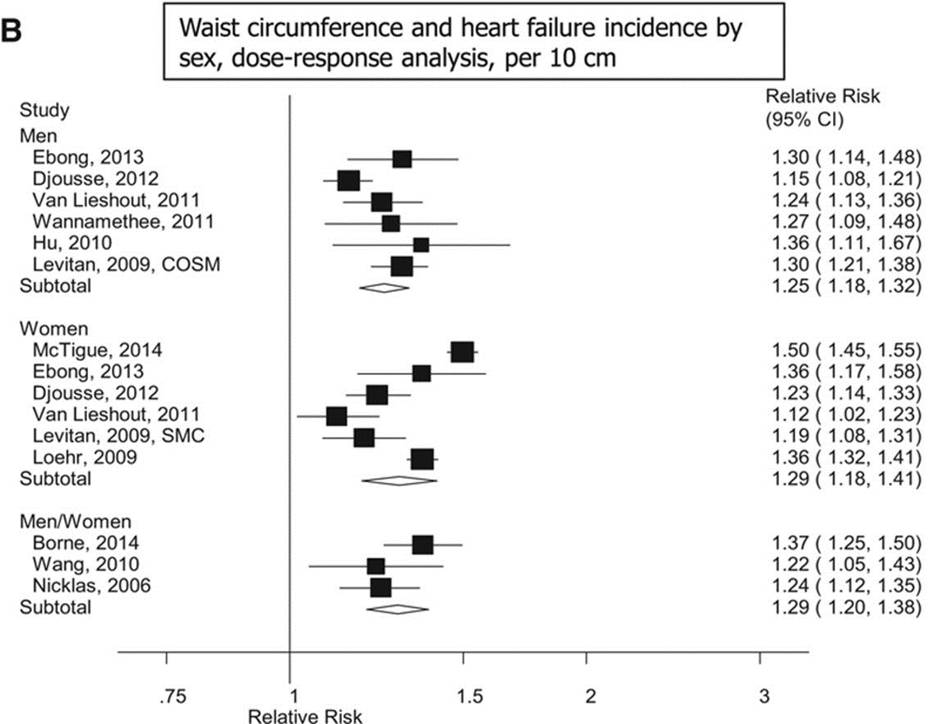
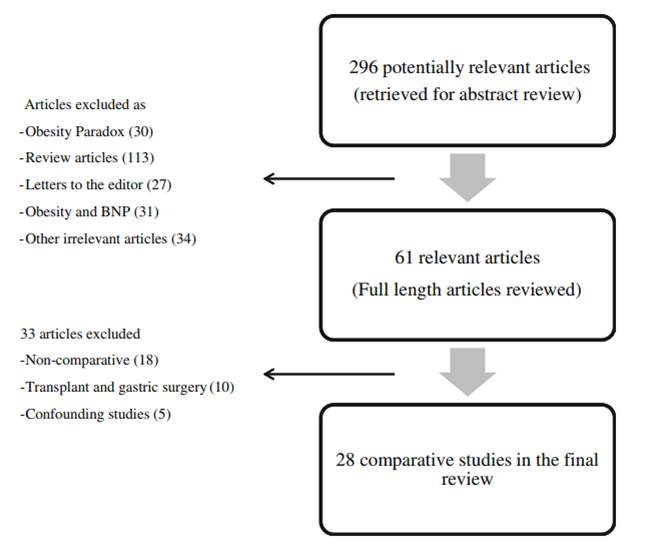
Body Mass Index, Abdominal Fatness, and Heart Failure Incidence and MortalityCLINICAL PERSPECTIVE
[7]
前瞻和回顾性队列研究巢式病例对照研究共28项
10 USA
1 Japan
1 Austrilia
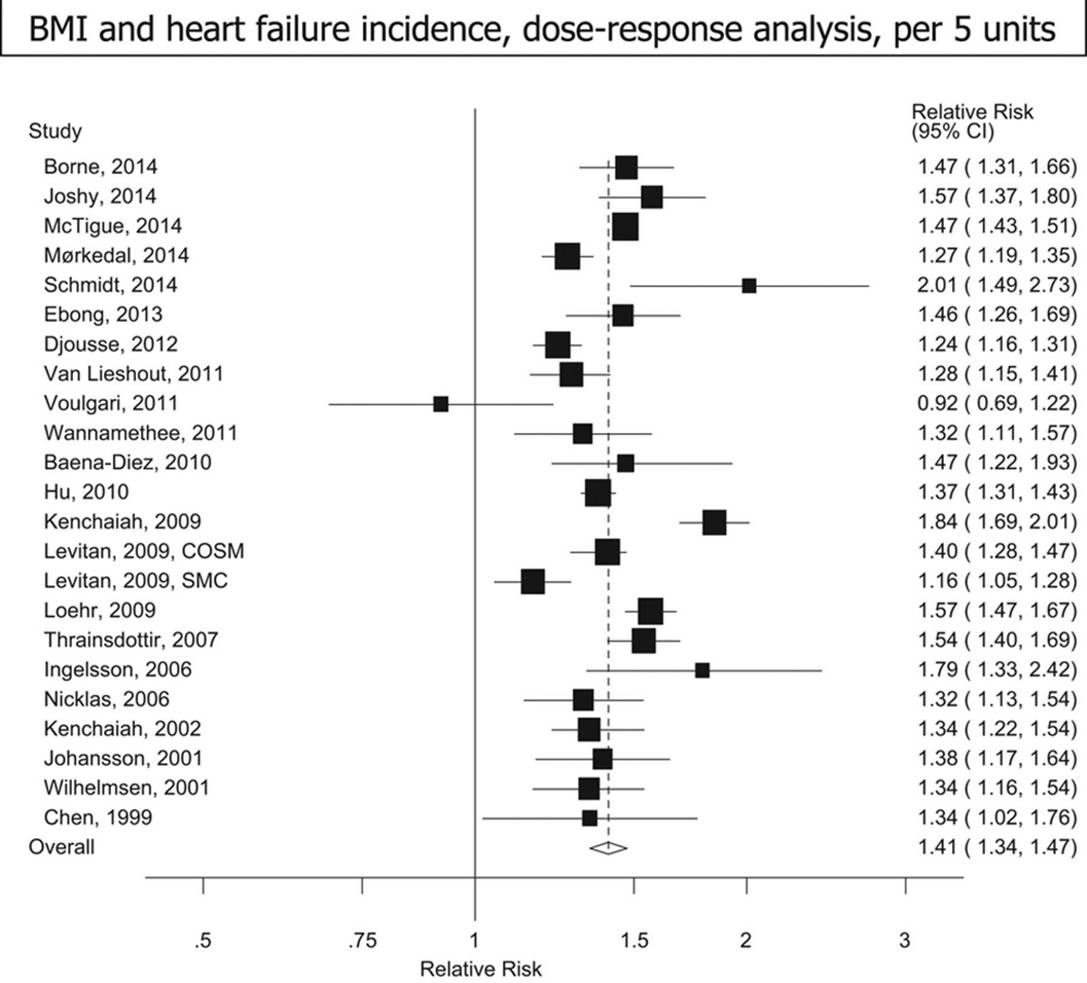
BMI增加5单位,HF发病风险比为1.41
[8]
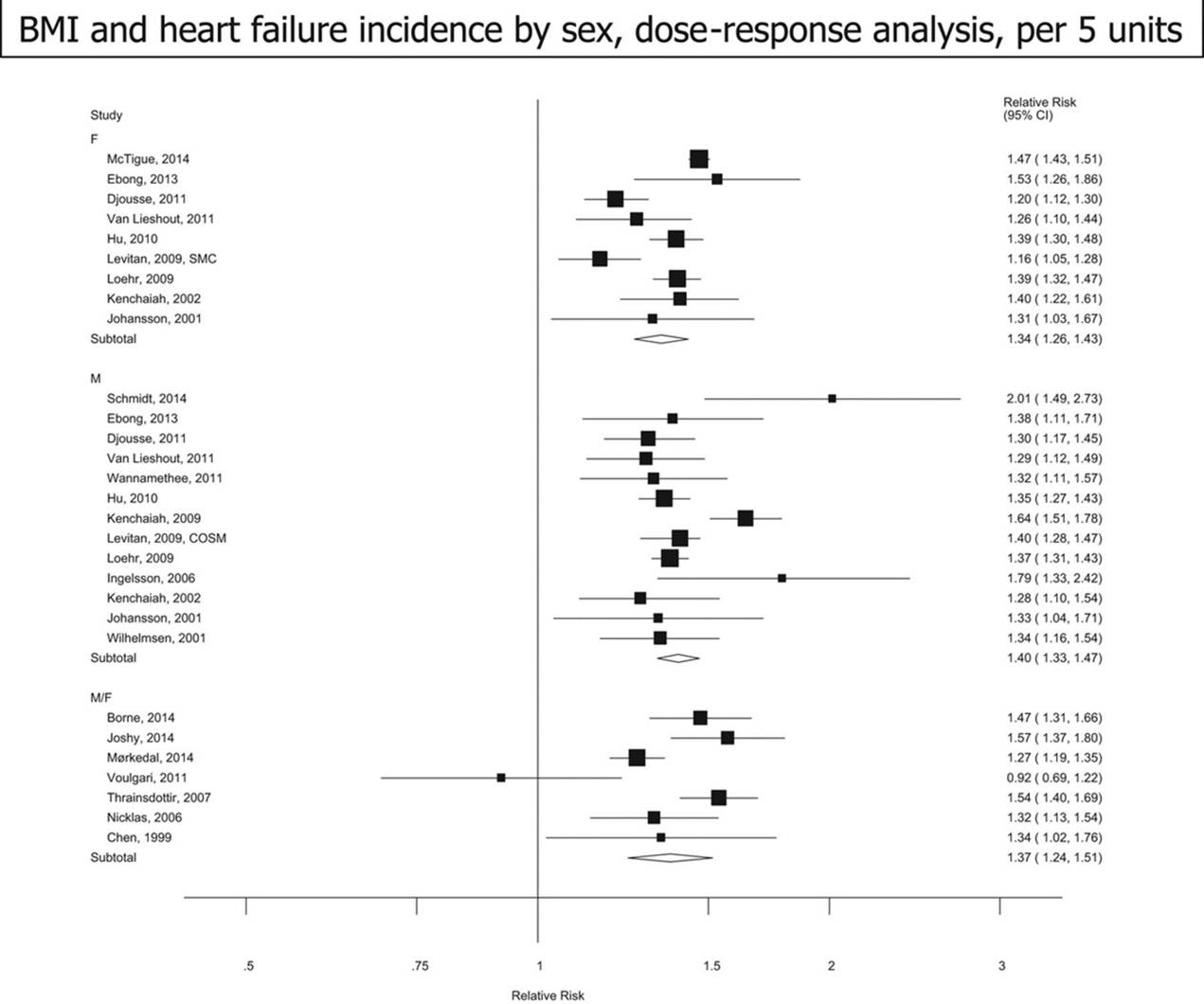
[9]
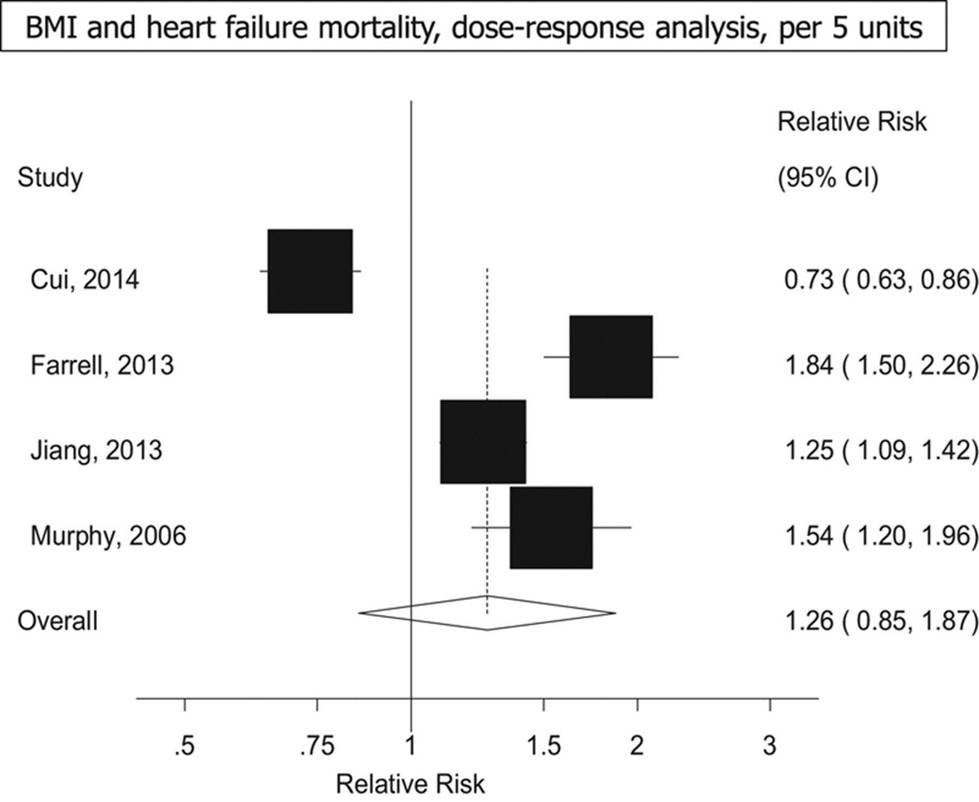
BMI增加5单位,HF死亡风险比为1.26
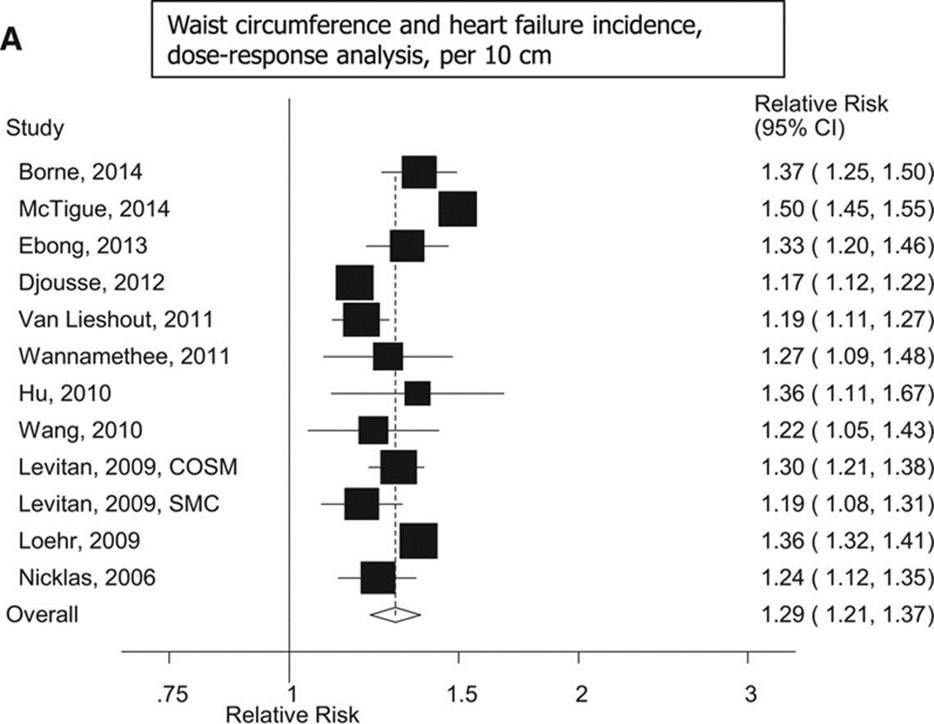
WC增加10cm,HF发病风险比为1.29
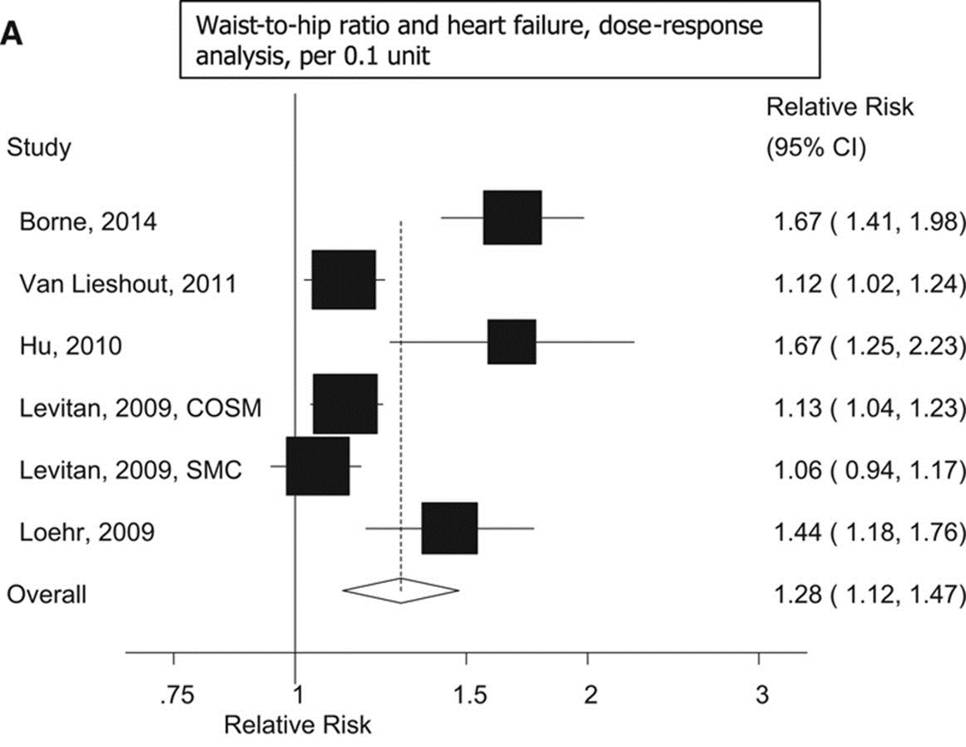
腰臀比增加0.1单位,HF发病风险比为1.29
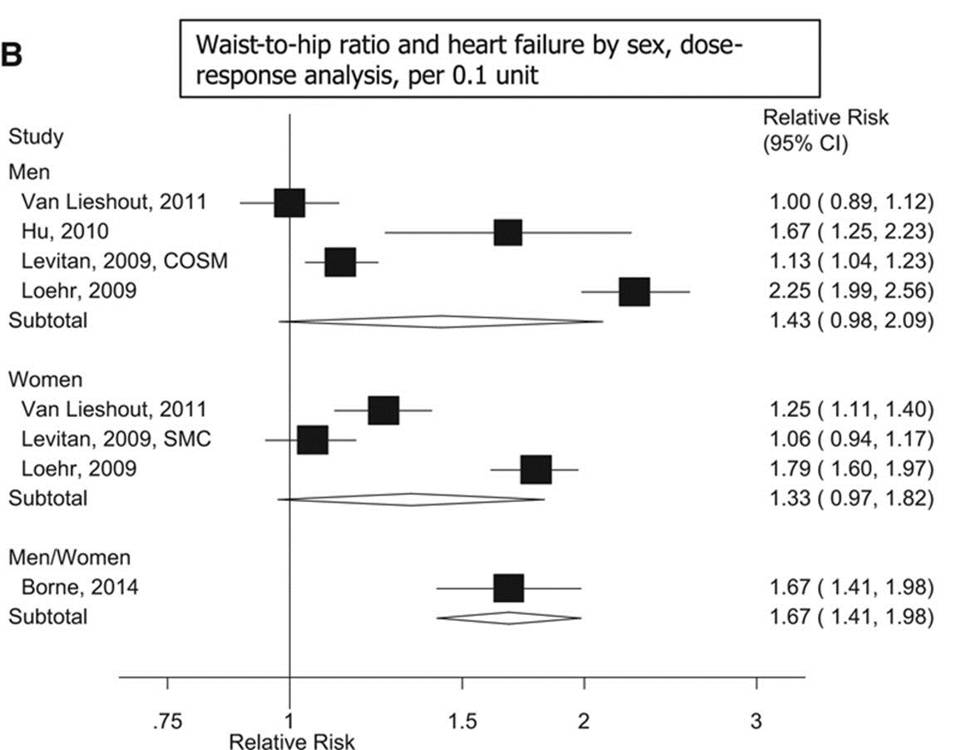
[10]
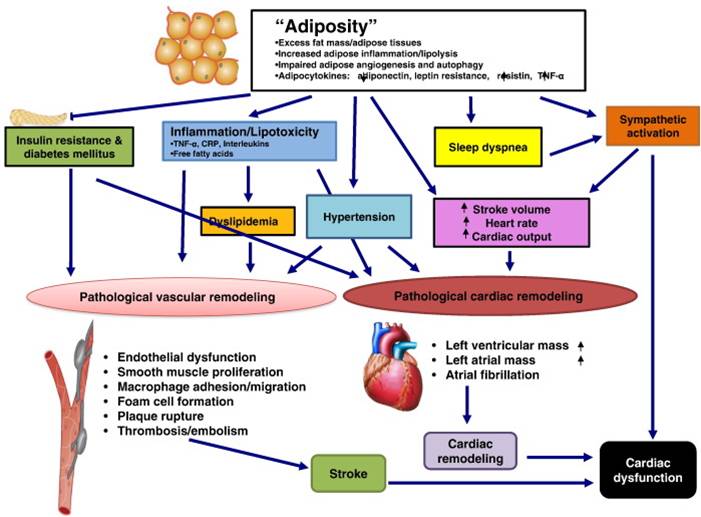
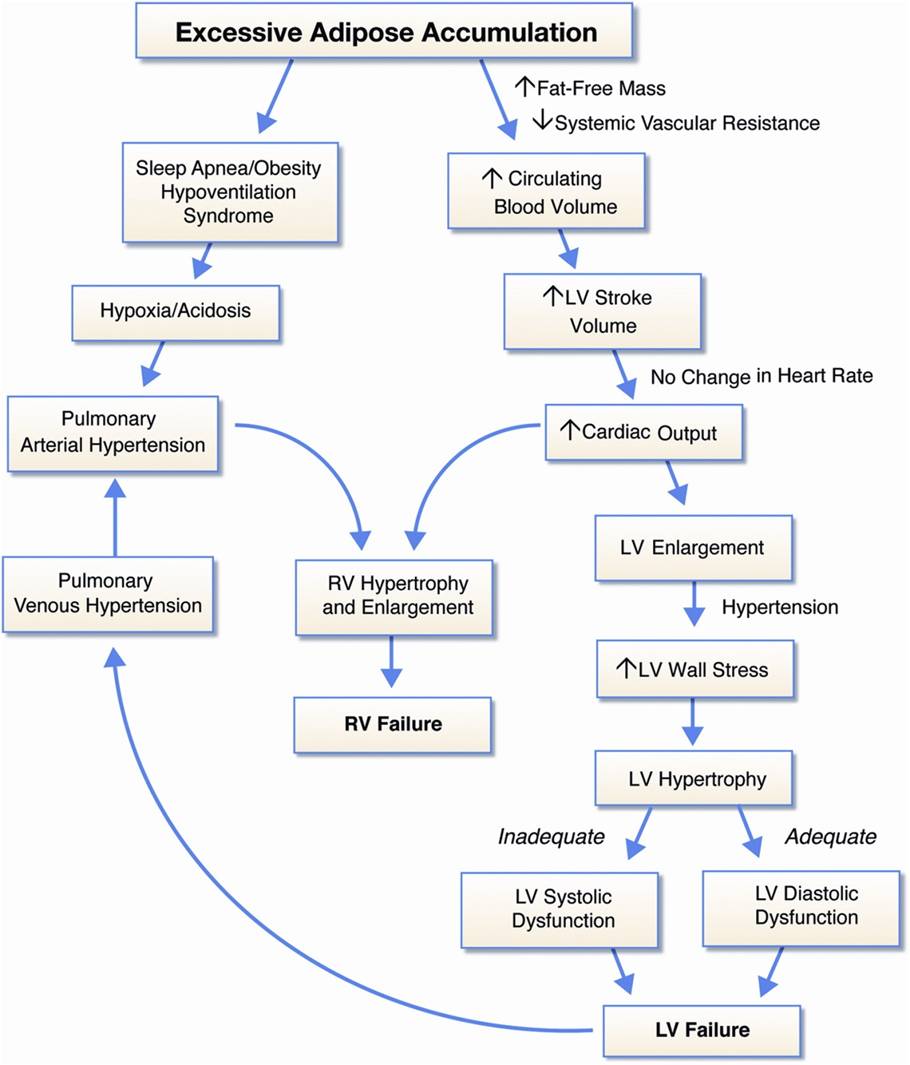
◆单纯性肥胖可引起血流动力学及心脏结构改变
◆但没有证据提示单纯性肥胖可导致收缩功能障碍和扩张型心肌病
◆肥胖伴左室收缩功能障碍的病人,应完善进一步检测,明确潜在病因
[11]
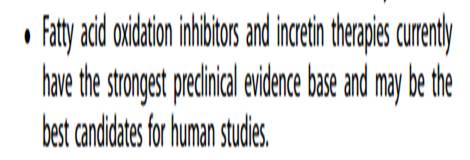
Should We Target Obesity in Advanced Heart Failure?
[12]
◆Obesity is a risk factor for the development of heart failure (HF), but has been associated with improved survival in patients with established HF.
◆Weight loss should clearly be recommended and supported for obese individuals without cardiac pathology to prevent cardiomyopathy development.
◆Morbidly obese individuals (BMI ≥ 40 kg/m2) aged <50 years with severely depressed systolic function and NYHA class III-IV symptoms should be considered for malabsorptive bariatric surgery at an experienced center. The goal is either improved systolic function and symptoms, or sufficient weight loss for heart transplant eligibility.
◆争议:Overweight and mildly obese HF patients (25–35 kg/m2) may be somewhat protected from cardiac cachexia and weight loss is not expected to enhance survival, but may offer symptomatic benefits.
[13]
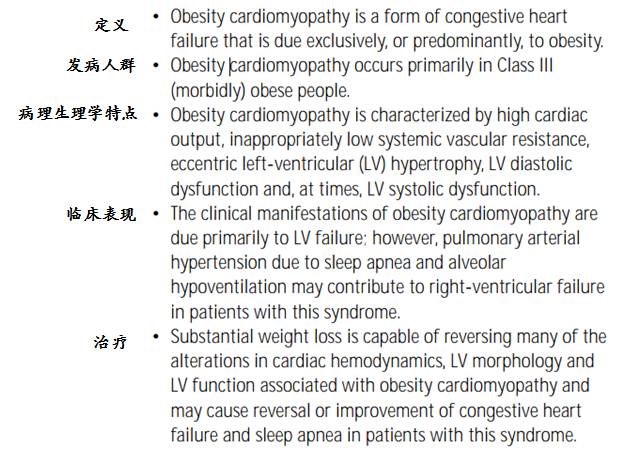
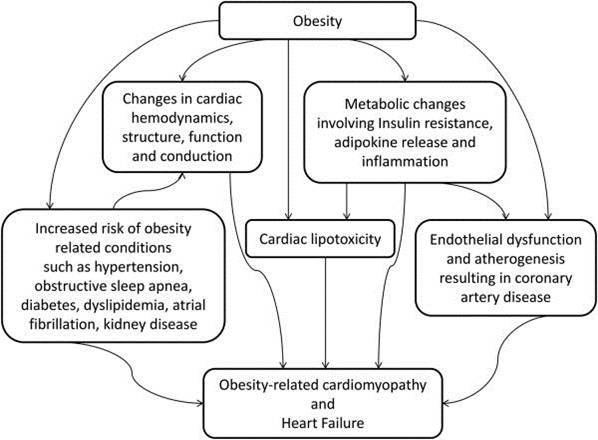
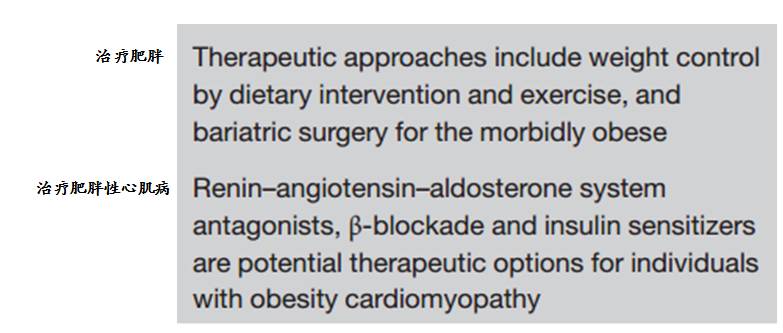
肥胖与肥胖性心肌病
[14]
[15]
[16]
◆脂肪因子介导的旁分泌疾病
◆可逆,心肌超微结构改变轻微
Reversible Cardiomyopathies:
◆Uremic:renal transplantationCirrhotic: liver transplantation
◆Obesity: bariatric surgery
◆Tachycardia-induced:radiofrequency ablation or pharmacologic therapy for rate or rhythm control
◆Stress-induced:supportive care
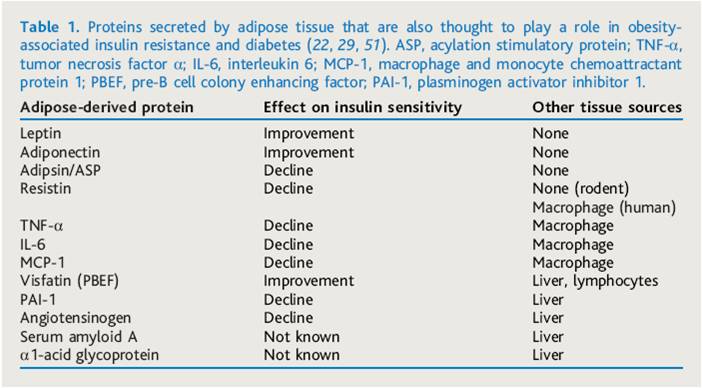
脂肪细胞分泌的蛋白质
[17]
[18]
◆Left ventricular (LV) hypertrophy in severe obesity may be eccentric or concentric
◆In uncomplicated (normotensive) severe obesity, eccentric LV hypertrophy predominates
◆In severely obese patients with long-standing systemic hypertension, concentric LV hypertrophy is frequently observed and may occur more commonly than eccentric LV hypertrophy
◆Whether and to what extent metabolic disturbances, such as lipotoxicity, insulin resistance, leptin resistance, and alterations of the renin-angiotensin-aldosterone system, contribute to obesity cardiomyopathy in humans are uncertain
[19]
参考文献
[1]IDF:国际糖尿病联盟;MS:代谢综合征
[2]J Card Fail,2010,16(11):880-887.
[3]J Card Fail,2011,17(5):374-380
[4]JACC Heart Fail. 2015 Nov;3(11):917-26
[5]Science 2013;341:856-858.
[6]Eur J Heart Fail. 2011 Feb; 13(2): 200–206
[7]Circulation. 2016;133:639-649
[8]Circulation. 2016;
133:639-649
[9]Dagfinn Aune et al. Circulation. 2016;133:639-649
[10]Heart Fail Rev (2013) 18:207–217
[11]https://doi.org/10.1016/j.amjms.2016.05.014
[12]Curr Treat Options Cardio Med (2014) 16: 284
[13]Expert Opinion on Therapeutic Targets, 2016, 755-766
[14]Expert Rev. Cardiovasc. Ther. 3(2),225-230(2005)
[15]Obes Res Clin Pract. 2014 ; 8(6): e540–e548
[16]International Journal of Cardiology 168 (2013) 144–150
Trends Cardiovasc Med. 2015 February ; 25(2): 127–128
[17]Transplantation Proceedings, 42, 3673–3678 (2010)
[18]J Am Coll Cardiol HF, 1 (2013), pp. 93-102
[19]Nature Reviews Cardiology 4, 480–490 (2007)
作者简介

齐康
医学博士,2012年毕业于北京协和医学院,毕业后在阜外医院工作,主要从事冠心病、心力衰竭的临床和基础科研,在国内外期刊发表论著3篇,综述1篇。目前在阜外医院心力衰竭中心进行专科医师培训。